Frontline Physicians on Coronavirus Pandemic
Below is the account of an interview with four physicians that are at the frontline of the coronavirus pandemic. This interview was conducted for Pakistan Link by Arif Mansuri, the President of PL Publications, the publisher of Pakistan Link and Urdu Link. As of the recording of this interview in late April 2020, coronavirus was continuing its spread across the world with around three million confirmed cases in 185 countries. For a video recording of this interview please visit www.PakistanLink.com/FrontlinePhysicions.
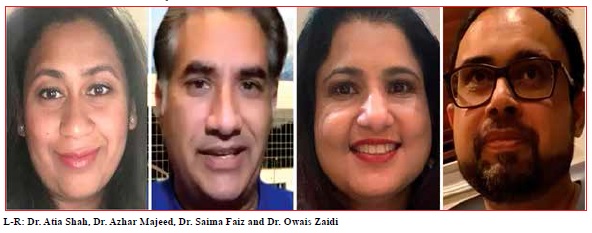
Pakistan Link: For a straight talk about coronavirus and to learn how to protect ourselves we have invited four doctors who are on the frontline of the coronavirus pandemic. They live and work right here in Southern California. Each of these doctors has been treating coronavirus patients on a daily basis. They have been watching patients recover and also unfortunately die from coronavirus. Now they will share their firsthand experience with this disease and give current and valuable advice on how we can protect ourselves, our family and our community.
First, I would like towelcome the panelists and introduce the panel.
First up, I have Dr. Atia Shah. She is a specialist of infectious diseases. She is an assistant professor at Department of Medicine at the University of California, Riverside. She is also the vice chair of the Department of Medicine at the Arcadia Methodist Hospital, California.
Next up, Dr. Azhar Majeedis an MD, MBA, FACP, FHM. His specialty is internal medicine and he is a hospitalist. He is on the COVID-19 Taskforce/MEC at San Antonio Regional Hospital. He is the president of the Southern California chapter of APPNA.
Next we have Dr. Samia Faiz. Her specialty is internal medicine and she is also a hospitalist. She is the assistant professor at the Department of Medicine in University of California, Riverside, and she's a councilor for DOGANA, the association of Dow graduates.
Last but not least, Dr. Owais Zaidiis a pulmonary and critical care specialist. He works at the San Antonio Regional Hospital in Upland, California.
Pakistan Link: Dr. Atia Shah, I would start by asking you that currently in the whole world about 200,000 people have died from coronavirus Covid-19, and there have been roughly three million infections worldwide as of now in the late April 2020. Out of this, 50,000 deaths and one million infections are in the United States.

I understand that the influenza virus, which is commonly known as flu, is also very deadly. In the United States we have the flu season from October through May, and according to CDC, this season, in this year we have had 30,000 to 60,000 deaths till the middle of March 2020. So, the flu virus is also very deadly. I would like to ask you what is the difference between the flu virus or the influenza virus and the COVID-19, what are the differences in symptoms, and why is COVID-19 so much more dangerous?
Dr. Atia Shah: Thank you for this opportunity to share with you our experiences. As you may know, both are respiratory viral illnesses, but what we are calling now COVID-19 or coronavirus disease is caused by a virus called SARS-CoV-2, and this is a novel coronavirus.
We are familiar with coronaviruses which, from what we have seen cause mild cold-like symptoms, but this is a novel virus. That means we have not seen this before. We are not familiar with it. We have seen similar things in the past like MERS which is Middle Eastern respiratory syndrome, or SARS in 2000, but this subtype, the SARS-CoV-2 is completely new to us.
Since it is so new, we don't have any experience of how to treat it. We don't have a vaccine for it, and we don't know how it's going to behave. As far as influenza, it's somewhat predictable to us. We know the viruses that cause it, A, B. We know that it comes in the winter season and by springtime it dies out, and we have a vaccine for it, and we also have medications to treat it, and we can tweak those medications as the virus mutates. But as far as COVID-19, it has completely taken us by surprise and we have no experience of how it's going to behave, nor any experience treating it or any protection from vaccination, which is why I feel that it has been much more deadlier as an unknown enemy to us.
I would like to share with you some differences between influenza and the coronavirus. Coronavirus definitely has much higher mortality rate than influenza and it also has higher infectivity.We assess infectivity by R naught (R0) number. It basically tells us how many people will be infected if one person becomes infected. For the flu that number is 1.3, which means one person who's infected, infects another 1.3 persons. However, for COVID-19 that number is at least 2.5 to three. That means any one person who's infected goes and infects three more people.
As far as the incubation period, the incubation period for flu is only one to four, so we know as soon as somebody gets an infection within four days they have symptoms, however with COVID-19 the incubation period can range from one to 14 days, and the incubation period mainly means the time from exposure to first symptoms.
But the problem here is a lot of time during this 14-day period people are transferring the virus without even knowing that they have illness, so essentially for the five days or six days before they're even aware that they are infected with the virus they are spreading it to others, and this is a very dangerous aspect of this virus which is not really so much so with the flu.
In addition, the hospitalization rate for COVID-19 is much higher. About 20% compared to 2% for influenza. Both cause pneumonias, but COVID-19 has definitely proven to be a more serious infection, which is why its case fatality, which means percentage of reported deaths among total cases is much higher than flu. For flu it's about .1, but for COVID-19 it's about 3.5%, so these are the reasons why COVID-19 has been much more deadly than the flu that we are familiar with.
Pakistan Link: Thank you, Dr. Atia Shah. Dr. Azhar Majeed, your specialty is internal medicine and you are a hospitalist. You see patients as an inpatient and outpatient, so you see the patients of COVID-19 at your office, outside the hospital, and also at the hospital. What is your experience managing this virus in the office and in the hospital, and how can one prevent getting to that stage to have to be admitted to a hospital?
Dr. Azhar Majeed: Thank you, Mr. Mansuri for having me on this panel of frontline physicians, and it's my honor to be here with all of you. First of all, I just wanted to say for our general discussion here tonight and probably for all the physicians, this is really informational, and it really doesn't constitute providing medical advice, diagnosis or treatment. I really want to remind everyone, please contact your primary doctor. Get the specifics for your health conditions.
Mr. Mansuri, regarding your question as to how weare treating these patients as in the office. Well as you know, the governor's stay at home order and the LA County Safer at Home program has been instituted now for several weeks. In fact, most offices are closed nowadays because they can't prevent the strict social distancing and the criteria that a large hospital could for example.
So we've actually instituted telehealth throughout our practices and outpatient. The patients are having video visits. We can see them in real time. We can get to them quicker and they can be safe at home. They do not have to travel. They are not exposed to anybody in the office or in their journey, and that's one of the ways that we've been working on it with the telehealth video visits.
To really get to your point of the issue of how to prevent hospitalization, well first off obviously if anybody has a serious medical condition, shortness of breath, chest pain and so forth, you need to call 911. You need to make sure that you get medical care. I do not want you to delay your medical care. The issue of getting to the point of when the patient needs to be hospitalized. Obviously, we have CDC's high risk criteria including age, including multiple medical histories and comorbidities as we call it, and obviously these patients need to be pre-screened and need to be directed to the appropriate facility.
How can you prevent it at home is really to follow the rules. Practice the social distancing, stay at home. I encourage all my patients, especially those over age 65, you really do not need to leave your house unless it's absolutely necessary. If you are an essential worker I understand, you have got to go, but most counties including here in Los Angeles have allowed the essential workers to glove up, mask up.And what you can do is what all the officials are saying and all the advice you've been hearing. Wash your hands with soap for at least 30 seconds. Avoid touching your eyes, nose and mouth with unwashed hands. Clean and disinfect frequently touched objects and surfaces. Cover your sneeze into your elbow, not into your hands. Wear a face mask.And we're a little bit late now, but those of you that did not get the flu shot to prevent influenza, there's still time and CDC still recommends getting that if you haven't done so this season.
Pakistan Link: Thank you, Dr. Majeed. My next question is for Dr. Samia Faiz. You are an educator and your specialty is internal medicine and you are also a hospitalist. You see the patients as as outpatients and as inpatients in the hospital. You are also an educator and teach medicine as assistant professor at UCR. I would like to ask you as an educator, what education are you providing your patients about Covid-19, how can you educate the community and what advice do you have for us? What should we be doing regarding the situation with this coronavirus pandemic?
Dr. Samia Faiz: Assalam-OAlaikum. Thank you so much for the opportunity to share our experience. I’m really happy to be here. As this pandemic has affected everybody, it is really important to educate our community and our patients.
I mostly see patients in an inpatient setting and not outpatient at all. Mostly educating my residents. While making rounds with my residents, I see really, really sick patients in the hospital. I see patients who are dying and the patients who are COVID-positive, and patients who are non-COVID-positive but are at high risk while they are in the hospital.
It is a really challenging situation in the hospitals. We educate our patients when they are discharged from the hospital to be safe. There are patients in the hospital who are COVID-positive and when they recover and when we discharge them, we have to be very specific with them about not to share a bathroom with other family members. Their things should be separate, their food should be separate, and their trash can should be separate. And then we dispose everything, and we ask their caretakers to really have strict precautions, hand washing, spraying the disinfectant on all the surfaces, and then hand washing before and after touching the patient's stuff.
So that is for the COVID-positive patients that we see, and then when they are discharged, we have to quarantine them. We have to isolate them from at least, according to CDC recommendation, about 14 days from the onset of their symptoms, and when they're discharged they should really distance themselves from others. Once the quarantine is over, they should still practice social distancing. Regarding non-COVID patients that we see in the hospitals, when they are discharged it will be the same as the regular community members as Dr. Azhar Majeed said and as Dr. Atia Shah said.
The community is really challenged right now. We must practice social distancing. People should at least stay away six feet from each other, and it is really, really important because when patients or normal population in the community are in the close proximity, they are putting themselves and others at risk.
We ask the regular community membersto wear a mask. A cloth mask is fine. The health care professionals in the hospital should wear a N95 mask and always protect themselves with personal protective equipment.At the hospital I usually wear gloves, gown, face cap and a head cap.Most of the patients in the hospital, if they're COVID-positive, are in one area of the hospital.
We are seeing new and new patients right now, so we want to educate the community to practice social distancing as much as possible still.The CDC said hat end of April would be the peak of coronavirus, but I'm seeing new patients now, and I feel that our numbers are increasing. We need to be very careful and we need to tell our community to practice social distancing, wear a mask, wash our hands, take care of our mail, take care of cardboard boxes, and continue all the precautions until this pandemic is really over and the restrictions are lifted.
Pakistan Link: Thank you, Dr. Samia. My next question is for Dr. Owais Zaidi. You are a lung specialist and you are seeing many lungs related complications. I’'d like to ask you, what is the acute respiratory distress syndrome, ARDS? And also, why are these viruses finding their way into the lungs, and what are some of the complications?
Dr. Owais Zaidi: Thank you for the invitation. So as pulmonologists we have been at the forefront of taking care of patients with COVID-19, and one of the main reasons the lung physicians have seen the severity of this disease is because the COVID-19 virus targets the respiratory system. That's how it gains entry into the human body. These receptors which let this virus in are found all throughout the body, but the virus, the way it gets in is it binds to these receptors to get inside our lungs.
ARDS is a syndrome where it causes severe inflammation inside the lungs, and this syndrome has been seen for a long time, and it's been associated with other diseases, however COVID-19 has really brought this syndrome into spotlight.
ARDS, causes leaking of the vessels because of inflammation inside the lungs which makes it difficult for the patients to breathe and their lungs fill with inflammation and water, and to overcome this patients breathe fast, they require oxygen, and a small minority of these patients end up going on the ventilators.
I would say about five to 15% of patients who have been diagnosed with coronavirus do develop this complication of respiratory failure, ARDS, and they require the support of the ventilator. Once patients go on the ventilator it comes with its own baggage of problems such as more bacterial infections on top of the viral infections. They can go into kidney failure, and we have also seen blood clots that are forming in patients who have been diagnosed with coronavirus and they end up progressing to respiratory failure, especially the ones who get on the ventilator.
Now I have to say that even though there has been studies or it has been noted that patients who end up going on the ventilator, they have a very high mortality. It's been written as almost 80 to 90% of patients who go on the ventilator end up not surviving. Fortunately, we have seen patients, about 50% of patients who go on the ventilator end up not doing well, but a lot of them actually do survive. A lot of them do get extubated, however they are taking a very long time to recover from this.
Pakistan Link: Thank you very much, and that's a very good news that you're seeing that more patients that are going on the ventilators are getting better, so that is definitely good news.
Dr. Owais Zaidi: Yes, and I do want to point out that at the beginning of this pandemic we were actually blindsided because we didn't know how this disease acts, what do patients present with and what are the complications we need to be watching out for. As we get to know our patients more, as we get to know how this disease works we're able to take care of these patients better, and the complications that are associated with this disease better, and hence we have better outcomes.
Pakistan Link: Dr. Zaidi, do you have enough ventilators?
Dr. Owais Zaidi: Fortunately, at our hospital, we didn't have any issues with ventilator shortages. There are some of my colleagues at other hospitals that did notice some shortages, but a lot of them were short-lived. That means that the shortages were short-lived.
Pakistan Link: Thank you for very valuable information, everyone. I'd like to ask you, Dr. Shah, I understand that there is no vaccine as of now, but are there any treatments that seem to be working? And, are there any medicine or food supplements, vitamins, something that one can take to prevent getting the coronavirus?
Dr. Atia Shah: As I had mentioned this is a completely new virus to us that we were not really prepared to address. That being said, as of right now there are no FDA approved treatments for COVID-19. Right now, the treatment is mainly supportive care which means supplemental oxygen, fluids if needed, managing the vent if they get onto that. However there have been certain drugs that have been tried in other places and we are going by that data which although is very small, which means we have very small samples for these patients, but there have been certain drugs which although not FDA approved are being considered and more and more information is coming out about them as we learn about them.
This has been the frustrating part of this pandemic, that we don't have clear cut guidelines and we are kind of making the guidelines with our experience and with what we are seeing, and also changing guidelines as we see side effects to drugs.
So, several drugs are under investigation for COVID-19. One of the drugs that is being considered and being used is chloroquine and hydroxychloroquine. This is not a drug that is new to us, especially people from India, Pakistan. It's an old antimalarial medication that has shown some in-vitro activity against the SARS-CoV-2 virus and early data has shown some promise. Then there is Remdesivir which is another antiviral medication that was developed to actually treat Ebola virus. It also has in-vitro activity against SARS-CoV-2 but is currently only being used on trial access basis.Then there are other drugs that came and were swiftly not thought to work, and these are antiretrovirals like lopinavir–ritonavir, but they were tried on some of the patients but not really found to be greatly beneficial. Other things that we are trying are convalescent serum plasma, which basically means that any patient who has recovered from this disease and has antibodies to this, basically they are trying to take out those antibodies and give it to the patients that are struggling with the disease in an effort to help that patient fight this virus.The other things that are being considered and used are immunomodulatory agents. So the way this disease works is a two-pronged approach. One is the activity of the virus which causes the damage to the lung, and in reverse it's also the body's ability to fight the virus which is causing a lot of the damage as well, so basically these drugs affect the immune response of the body to try to prevent further damage. Unfortunately, none of these therapies are completely proven to be efficacious, and there are still trials and new information coming out about managing this every day.
As far as the nutrients, I think the biggest thing at this point right now is trying to prevent the illness. Keeping healthy, exercising, but some things that people are considering as far as supplements are zinc. Zinc has been associated with the body's ability to mount an immune response, so some people feel that taking some zinc supplementation, and I've also heard this from physicians who are using this, especially if they're on service, they will take some zinc tablets to try to have an adequate immune response. Other things, vitamin C which has been associated with a lot of other things included fighting sepsis, that has an antioxidant properties which limit inflammation, however I can tell you that oral vitamin C is not enough, and what has shown some benefit is IV vitamin C. The other things are vitamin D. It has shown that good levels of, adequate levels of vitamin D help fighting, help with inflammation and prevent tissue damage in the body, so these three supplements have shown some benefit, but other than that I think right now we are still in the trial and error phase of trying to deal with this virus, which is somewhat unfortunate.
Pakistan Link: How much of each of these vitamins do you recommend, like the vitamin C, zinc and D3? And what about the echinacea. What is the dosage that you recommend of each of these?
Dr. Atia Shah: As for the vitamin D, I would suggest that before taking supplementation for vitamin D it's best to get your vitamin D levels checked. Most of us in California are lucky that we have average sun exposure, but nevertheless so the dosing will be based on your deficiency and how deficient you are, so I wouldn't say that it's a fixed dose.For zinc it's about 50 milligrams per day. We do not want to take overdosage of this because it can have effects on the kidney, and for vitamin C most people usually take about two tablets a day, but again the efficacy of all these supplements is not proven.
Pakistan Link: Dr. Azhar Majeed, I would like to ask you what happens if I feel that I have coronavirus. Who do I call, and if I feel that I may be infected with coronavirus, can I get tested? Do you have any resources for us for that?
Dr. Azhar Majeed: Sure. That is a very common question among the patients. They'll call, say, "Hey, I think I've been exposed." So I always ask them, "How? If you haven't been out of your house, what have you been doing?" Number one, you got to stay at home. The message has not been exhausted enough and I think most people are doing that but we really need to follow that.
But if you think you've been exposed, number one the CDC guidelines currently still are you need to quarantine yourself for 14 days. Remember, the vast majority of us are going to have minimal to none symptoms, so there's only going to be those that have symptoms are in the most serious aspect of it later, but most of us will have minimal or flu-like symptoms.
Now, once you quarantine yourself what you need to look out for. The big ones, cough and shortness of breath. Any difficulty breathing you need to call your doctor; you need to find out. And at least two of the other symptoms as recommended by CDC including fever, chills, repeated shaking with chills, headache, sore throat and new loss of taste or smell.
Now if you had any of these emergency warning signs you need to seek medical attention immediately. You need to get to the nearest hospital and so forth, especially with trouble breathing, persistent pain or pressure in the chest. New confusion or inability to arouse. Bluish lips or face. Of course, the list isn't exhaustive. If you're not feeling right, if you think something's wrong, get yourself some attention.
Your other question about testing, and I'm glad you brought that up, Mr. Mansuri, especially here in LA County, now nationally and on state level we've been a little bit behind on testing. We can't get everyone that wants a test a test currently, but for the vast majority of us now, especially here in LA County, testing has been ramped up significantly.
I would recommend that you call your local hospital and ask them. Geographically LA County is a really large area. We have over 15 drive-through sites currently. Before you had to go online and get an appointment and so forth. You still do. We're still prioritizing obviously for those patients who are hospitalized, health care workers, workers living in congregate living settings, first responders with symptoms, residents in long-term care facilities and the nursing homes, including prisons, shelters. These are obviously a higher priority. Also, people who are older, over age 65 with multiple comorbidities, multiple medical conditions, and anyone with symptoms. Anyone with symptoms including the fever, cough, shortness of breath, the ones that I mentioned before, they should be able to get tested.
If you can’t reach your doctor, go to the local county health department. One of your best resources and I'd really like to get this out to the community, is your local county health department. LA County, Orange County, San Bernardino, Riverside. Wherever you live here in Southern California, I'm very familiar with LA County's Health Department. They have great information for patients. Great information on where the drive-through testing centers are, and I really encourage everybody to look that up, please.
Pakistan Link: You mentioned fever. How much should the temperature be before one should start getting worried?
Dr. Azhar Majeed: Many of these COVID patients, and I'm sure Dr. Shah and Dr. Faiz and Zaidi can corroborate, have multiple fevers over several nights. And yes, one of the key hallmarks is high degree of fever, but if they're not having the secondary symptoms, shortness of breath, confusion, chest pain, they can take the fever-reducing medication. Check in with their doctor early and quite frequently. Most physicians, large practices, have video visits, you have your TeleVisits. Please get in touch with medical personnel.
Pakistan Link: Thank you, Dr. Majeed. Dr. Faiz, I would like to ask you how much socializing can we do? Is there any socializing that's permittable and how long should we stay at home, and also I'd like to ask you about what precautions we should take when we are staying home like how to clean the boxes, packages of food and other things that we are handling while staying at home?
Dr. Samia Faiz: We must inform the community to stay home as much as possible. I know everybody is tired. It is really, really difficult right now. I see more and more people going out of home, both in Riverside County and Orange County. I practice in the Riverside County and live in the Orange County. I can understand that people are really tired of staying home. They want to go out. They want to have fun. I've seen more people going out and it's dangerous at this time, because there's a chance of resurgence in the community. There are new people who are just getting infected. The more socializing that we do, the more harmful it will be and we may end up requiring everybody to stay home for much longer.
The families can go out.They are allowed to walk in their own neighborhood. They can go out together, but not with other families. When people do go out they must observe social distancing and stay away from each other at least six feet away. But I really don't think that social distancing is really possible in large group gatherings. We have seen outbreaks with the different large gatherings which increase the chance of people getting infected, and then we are putting everyone else at risk that includes people around us, people in our family, people who arein the community where we work. Some essential workers, people who are working like truck drivers, people working in the supermarkets, if they start going out and hanging out in a park with other people they may infect many other people.
Many of these people may be asymptomatic. They may not show all these signs of shortness of breath, fever, or cough. They may not have all or any of these symptoms, yet they may have been infected. It is extremely dangerous as these people can still infect others. So the social distancing, staying six feet away, staying home as much as possible is the basic key.
We are asking everyone to use masks in public. Cloth mask is good for all the communities. The health care workers should wear N95 mask and as well as gloves and other protective equipment that is available to us in our respective facilities. So that is important even in the hospital. Even outside the hospital we should really practice social distancing.
One word of advice, we have to clean all commonly touched surfaces. Whichever things are touched more, like our kitchenutensils, the bathrooms, the doorknobs, everything should be cleaned at least three times a day. That's what I think. If the surfaces are not properly cleaned you may be enabling infected surfaces to spread the disease.
Also what all of us are doing is that we are touching our mouths, our nose and our eyes frequently. We do that all the time without even be aware of it. I just would like to tell the communities not to do that as much as they can avoid it. I know it's almost impossible to do but we all should try to be conscious about it and make an effort to avoid touching our face. This is a serious disease. This is a serious pandemic. We have to be careful for everybody's sake. For our own sake, for our loved ones' sake, for everybody else sake so that we can prevent the spread of this disease, maybe can prevent a resurge.
So the surfaces should be cleaned. When we go out social distancing is important, and wearing a mask is good. As much as possible, we must prevent the spread of this disease.
Pakistan Link: Thank you so much, Dr. Faiz. Now next I will ask Dr. Zaidi, are there any medicine that one can take or is there anything one can do to prevent their lungs from getting damaged? Any supplements, medicine, exercise to ensure that the lungs don't get in a shape where a ventilator is needed?
Dr. Owais Zaidi: Well I think I'd just like to say or echo what Dr. Shah had said earlier. Anecdotally we know a few things that might help avoid getting infected with coronavirus, however none of these medications have been proven. Vitamin C, vitamin D and zinc. These are possible preventative measures one can take. I myself take vitamin C daily, and I don't think we're at that stage in our knowledge to suggest anything that would prevent us from getting any of these viral illnesses, especially coronavirus.
Pakistan Link: I'd like to ask a question of all the panelists. I'd like to know what prevention are you doing personally? I know that at the hospitals and at your places of work you take precautions to not get infected, but what do you do at home? How do you prevent yourself and your family from getting infected?
Dr. Atia Shah: I can share what I do. Since I have kids, I have parents who live with me and that is for any health care provider the biggest worry at this point which is, carrying the virus to our loved ones, that is what we would want to avoid the most. I can tell you that we are hypervigilant at this point in the sense that we are very cautious.
When I go to work in the morning I leave from a separate entrance through the garage and make sure I take all my things. I make sure when we are in the hospital we are following all the procedures. I mean the day has added extra two hours just because we're donning, doffing, washing up, cleaning after every patient that we see, washing our hands stringently and then we are wearing scrubs.
When we are coming home, I make sure that I don't enter the house from where everybody is. I enter separately. The first thing I do is I empty all my pockets, leave everything in the garage. I make sure that I do not meet anybody till I've gone in and taken a shower. I take off my scrubs, take off my lab coat, make sure I put it in the washer right away, and I'm cleaning my goggles. I have stopped taking any extra things with me like folders, keys. I am constantly sanitizing my hands to the point that they are becoming so dry.
The other things that we are doing at home too, I have separated an area for myself. I have one bathroom, one room that I am just using. Even at home although we are meeting family, I'm trying to maintain a social distance with my parents. I see them from far. If I have something close it's FaceTime. Everybody including my five-year-old now gets his bedtime story through FaceTime, so these are the things that we are doing because there is a lot at stake here for us.
Pakistan Link: These are certainly very tough times. Anyone else care to share what they do to ensure their family is not exposed to coronavirus?
Dr. Owais Zaidi: I kind of do the same thing as Dr. Shah is doing. I'm wearing scrubs to work every day, and when I come home, I come through a separate entrance, through garage. I get rid of my scrubs daily and put them in the washer, and I try to stay away from kids as much as possible. So yes, we just have to be very careful.
Dr. Azhar Majeed: To add to the others, all of us being essential workers and frontline people taking all precautions and following the common advice of the governor and the county. I have teenagers and older children and I do not let them go out to do any grocery shopping or unnecessary trips. We have someone to do that. We are trying to order stuff more often. Exercising at home. One thing I wanted to mention, and I think the governor said it last night, the coronavirus does not take the weekends off. We can't have thousands of people going to the beach on the weekend. We need to follow this stay at home order. in order to really minimize the spread of the virus and to flatten the curve.
Pakistan Link: To follow up on that I’d like to ask you that despite the high number of cases and fatalities, several states are going ahead with their plan to restart their economies, even though the United States does not have the kind of testing infrastructure that experts say is necessary to open up. What in your opinion will be a good time to open up the United States, or when will this be over? When will you feel safe to take your family to a restaurant or a movie without fear?
Dr. Samia Faiz: I feel at this time we should really be cautious and follow the CDC guidelines. We should really practice social distancing. We should not really go out to the restaurants. I know the beaches are open. The restrictions are lighter in some of the states, but we should not really take it lightly. We should really, really still practice social distancing as much as possible. It's for our own good.
We can't feel safe right now. This is a new virus for us. This is a new pandemic. We don't know when it is going to be over for sure, so at this time even though some of the States may be opening up, I feel that we have to still practice social distancing and stay away from larger crowds.
I agree with all the other doctors, Dr. Shah, Dr. Majeed, and Dr. Zaidi about the precautions we must take. The coronavirus pandemic has added two hours to my daily routine. I have to put everything in the trash when I come home. There's a separate trash can in my garage. There's a separate laundry basket in my garage. I leave things in my car instead of bringing them in to the house. Even if I bring any food or any mail in my home, I clean it up multiple times.
I know people are frustrated, including ourselves. For a few more months I recommend we must practice social distancing and be very careful. Then, I think we’ll have a better chance of survival and we may not see a resurgence of this disease.
Pakistan Link: When will this be over? Are we going to have to continue to quarantine forever until the vaccine is discovered? What do you see in the future regarding this disease?
Dr. Azhar Majeed: That is a good question. The life as we know it is not going to be a flip of a switch and we're not going to be able to have big parties and have all these people over. I think we're going to have to get used to a new normal. No handshaking. Maybe eventually when restaurants open very minimal people inside. Maybe your servers will have to wear gloves and masks, and so will you. Maybe there will be temperature checks. I mean I think until eventually a vaccination and a curative process is taking its place there needs to be some steps in order to protect the public.
Pakistan Link: Is this ever going to be over? After COVID-19 are we going to see COVID-20, COVID-21?
Dr. Atia Shah: I would say that we have seen pandemic before. We have seen SARS, we've seen MERS, so the infectious diseases and pandemics have been a big part of our past and are probably going to continue to be. What we should learn from this pandemic is it has exposed our weaknesses and we need to try to make ourselves stronger in those areas.
Most of the time the pandemics eventually pass. They become more contained or they, like the flu, are seasonal and pass off with time, or we develop better tests or have vaccines, so I have full hope. I think we need to be patient. We need to give it at least 12 months to see where we are headed, but I'm hopeful for our future.
Pakistan Link: Are you getting enough support from the community, and what can the community do to help you?
Dr. Owais Zaidi: I think we have seen a lot of outpouring of support from the community. I have seen community members bring in things such as extra masks. Some of the businesses have donated gloves and masks. Some of the community members have been providing lunches for the nurses in our hospital who have been working long daily shifts for seven, eight days in a row which can take a toll on our nurses and their families.
There have been people who have organized food drives for people who are unable to go out and make a living and earn for their families because of the social isolation and quarantine, so yes, I've seen plenty of community support.
Pakistan Link: Dr. Majeed, you are the president of Southern California Chapter of one of the largest association of Pakistani community in the United States, the Association of Physicians of Pakistani Descent of North America (APPNA). Please tell us how APPNA is responding to the current situation and what role it is playing?
Dr. Azhar Majeed: Absolutely. APPNA has been actually very active from day one with an aggressive fundraising community support program both for our members, our families, our communities here in the United States and also in Pakistan. If you go to the APPNA website, you’ll see that APPNA has launched a very significant campaign. In fact, just yesterday APPNA had a pretty impressive telethon on one of the local channels raising funds again. From what I understand, over three quarters of a million dollars have been raised by APPNA in PPE not only for here in the United States but also for people and the health care providers in Pakistan.
They have also done a lot of community event just like you're doing tonight hosting and educating, and so I believe that they've done a very good job on the forefront. Not to mention partnering with all the local organizations even in Southern California, whether it be food drives, PPE, and other such activities. The level of response of the community, not only the Pakistani American community or the Muslim American community but all the community has been really resounding and really quite humbling, because the people have really opened up their hearts and their wallets for a good cause to help their neighbors and friends.
Pakistan Link: My hat off to all of you. You're doing an incredible job. You are serving the humanity and providing selfless service. You are putting your life and your family’s life on the line and I pray that may God protect you and your family and keep you safe.
I'd like to ask you just as a personal question, knowing what you know now, about the coronavirus infections and knowing that so many doctors and nurses and health care workers have been infected and have lost their lives throughout the world, had you known this when you entered the medical school, do you think you would have chosen to become a chartered accountant or engineer instead?
Dr. Atia Shah: I would say that as I mentioned, infections and pandemics are not something new. I think we were very well aware of what we were getting into and we still chose this line. And honestly, other people look at us as heroes, but right now looking at all the suffering, the pain around us, we almost feel defeated.
As doctors, we are somewhat perfectionists. We like knowing exactly what we are doing and how best to do what we do, but this virus has caught us at a weak time when we are not exactly ready, but we are getting there. We are trying to come up with new things. We are trying to modify our strategies as we see results, and not for a second do I regret being a physician. In fact, I think tough times bring out the best in people and communities, and we really now have appreciation for the things that we used to take for granted and I think we are all going to come out stronger from this.
Dr. Samia Faiz: Yes, even though I believe we are doing a good job under the circumstances, working with what we have, we don't know much about the virus, and we were not prepared for this pandemic, but we are willing to sacrifice our lives or be together in this pandemic as a health care worker. So, I still would be a health care worker no matter what and try to educate as well.
So my job is not just to protect myself, and the doctors around me but also the residents. I have to be a role model for the residents. They have chosen this profession. They are new in this profession and my job is not to instill fear in them but to provide them the best education and to teach them to rise above the norm. We have to fight this together. We have to teach our communities. We have to stay strong during this time and be a role model. Not only just a health care provider, but a role model for other people, so that they stay calm too.
Also, I want to say that as a councilor of the Dow Graduates Association of North America (DOGANA), we are spreading our recommendations, the CDC recommendations to our community. The other guidelines which are available in university hospitals in US, we are educating Pakistani people about that and giving lectures and spreading the word so that globally we are proficient in spreading the current knowledge about the disease and trying to make sure that the guidelines are effective everywhere else also.
I have also seen so much community helping us out. Not only American community, but all over the world. I think that the world has come together to fight this disease. There are lots of organizations, Muslim organizations and others that are doing a great job.
Pakistan Link: Dr. Majeed, would you care to say something about this?
Dr. Azhar Majeed: I think all of the speakers have eloquently put it. The bottom line is we are in this together as a community. As neighbors, as friends, local communities, our cities, towns, counties, and if each of us can do our part I think we're going to be stronger. I applaud Dr. Shah's sentiment that she has hope, and I think we're going to come out of this stronger, and Insha Allah, God willing, I think by taking care of each other, taking care of our families, our friends and our neighbors, one step at a time we're going to get through this.
Arif Mansuri: Thank you very much everyone for a very informative talk. I would like to thank you for joining us today. This is month of Ramadan and it's late night so I really thank you for taking the time out to join and to educate the community. But more importantly I would really from the bottom of my heart like to thank you all for doing what you are doing, and lots of prayers and love to you guys. You are doing a noble job, this is incredible. We wish you all the best. We pray that may God protect you and your families and keep you safe. Thank you so much. Take care of yourself.
-----------------------------------------------------------------------------

