
Older Adults Still at High Risk for COVID
By Mark Hedin
“You might be done with Covid, but Covid is not done with you.”
So said Denny Chan, directing attorney with Justice in Aging, at a press briefing co-hosted by the California Department of Aging on June 29 to address the high risks older adults still face from COVID-19 and what steps will protect them.
Joining Chan were Department of Aging Director Susan DeMarois, Dr Susan Tartof, an infectious disease epidemiologist with Kaiser Permanente Southern California, and Roberto Velasquez, President and CEO of the Southern Caregiver Resource Center.
“From the outset of the pandemic and still to this day,” DeMarois said, “older adults have been hardest hit — 70% of all Covid deaths in California are people 65 and older.”
“So, we need your help in communicating the value of vaccines and boosters and testing-to-treatment for this population.”
Tartof shared research relevant to people of all age groups, such as new evidence that the biggest benefit of being vaccinated is not preventing infection but preventing severe outcomes from infections.
Vaccines wane in effectiveness – need boosters
Booster shots, she said, are proving more effective than the original vaccination doses.
But even the heightened level of immunity provided by a booster wanes over time, she said, and researchers now recommend additional boosters.
“Really, six months after a vaccination, you’re down to like, the protection you’d have from one or maybe none. That’s what drives the booster recommendation — They’re not providing the same protection that they did when you first got them.”
This waning is more acute in “immunocompromised” people, Tartof explained, which includes people, often seniors, facing an array of challenges such as leukemia, lymphoma, HIV, AIDS, stem cell or organ transplantation.
“It’s really important to protect yourself by staying up to date and to try to keep track of what current recommendations are.”
“It’s confusing,” she admitted. But, she said, “another thing I do is study long Covid. Those very debilitating symptoms are actually pretty much impossible to treat,” she warned.
“Every time I feel hesitant, I just think that I’m more willing to take risks with the vaccine, which are actually very minimal compared to the risks of long-term.”
Of those California seniors lost to Covid, 45% were Latino, more than twice their 22% of the population aged 65 to 79. African Americans, 5.5% of that age group, experienced an 8% death rate, Chan said.
Statewide, more than 80% of older adults have been vaccinated, 70% have had one booster, almost 30% have had two. But these statewide figures do not reflect regional differences, Chan cautioned.
“We can’t have a one-size-fits-all approach to getting people vaccinated. This is long-term work for the safety of all the older adults in our state.”
The rate of positive tests for Covid in California stands at 13.2%, probably an undercount, Chan said, but still 1.5 percentage points higher than the week before. And with 3,100 people currently hospitalized, he said, we’re back to the level we were in March, when Omicron spiked.
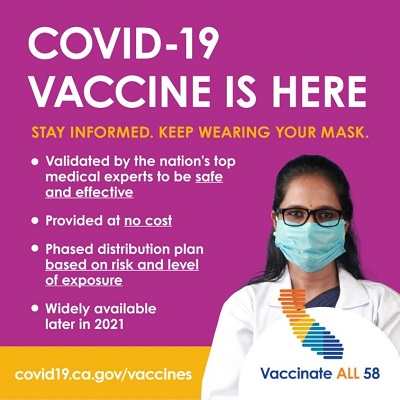
There’s plenty of vaccines
But there’s good news too. Unlike the early days of vaccine availability, he said, “We have plenty of vaccine,” so the days of rationing are over.
“We also know that vaccines work,” he said, and cited state data from May showing that people without vaccines are five times more likely to get Covid, seven times more likely to be hospitalized for it and 10 times more likely to die than those vaccinated and boosted.
Vaccines are being approved for more age groups, and there’s a potential for more specific vaccines targeting variants as they emerge, Chan noted.
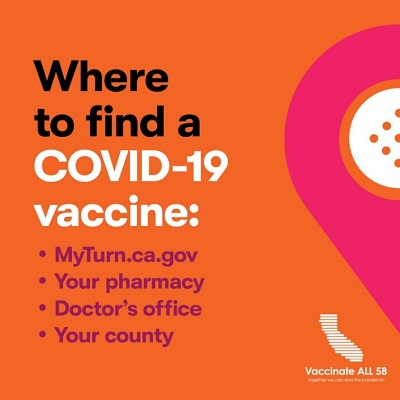
Also, he said, “access is easier than ever before,” with systems in place to vaccinate people at home, if necessary, that can be obtained with or without internet or cell phone access.
Free transportation or in-home delivery of vaccinations and boosters can be arranged in multiple languages by calling 1-833-422-4255. On the web, go to https://myturn.ca.gov/ , DeMarois said. The site covid19.ca.gov also has information and scheduling help available in dozens of languages.
Caregiver support
The state has 11 caregiver resource centers (CRCs) ( www.caregivercalifornia.org ) (1-800-510-2020, multiple languages) offering an array of free services to support those caring for people 60 and older or for adults with cognitive impairment issues.
Velasquez’s Southern Caregiver Resource Center is focused on San Diego and Imperial counties, where people 60 or older were 86% of the 5,000 Covid deaths recorded.
Of Velasquez’s care-provider clients, he said, more than 70% were spending more than 40 hours per week providing care and got no paid help. They self-reported fair to poor and worsening health, moderate to severe depression and loneliness.
“Caregivers usually don’t want help for themselves,” he said, but when Covid hit, the challenges of social distancing eventually led to increased calls for help in the form of the “respite services” CRCs can provide.
For his CRC’s 516 family caregivers, it came to a combined 192,600 hours in one year, Velasquez said.
“You have to get them to think that they’re helping their loved one, even though they’re helping themselves.”
Beware complacency
“For me, the most worrisome thing is how everybody’s become a little bit more complacent. Masks are not being worn on a regular basis. People are just tired. They just want to say, ‘Covid is over, let’s just do what we do.’”
“We really want to encourage individuals and families to consider safely re-entering settings where they can share meals, participate in activities and have multidisciplinary healthcare teams supporting them.” – Ethnic Media Services

